The shortage of respiratory ventilators has gotten a lot of engineers interested in how to make medical devices. Though requirements have been relaxed during the pandemic, there are still numerous hoops to jump through.
On March 24, the Food and Drug Administration dropped some of the provisions to be met before firms can begin making respiratory ventilators. These provisions are well known in the medical industry but may be unfamiliar to those in other manufacturing areas. For those interested in gearing up to produce these devices, an overview of the suspended requirements and those that are still in force may be illuminating. Despite the relaxed standards, it may be fair to say that the manufacture of medical devices is still not for the faint of heart.
The key provision that the FDA waived on March 24 was for what are called current good manufacturing practice (CGMP) requirements. These are spelled out in an FDA document titled 21 CFR Part 820, also known as the Quality System Regulation (QSR).
CGMP regulations govern the methods, controls, and the facilities used for designing, manufacturing, packaging, labeling, storing, installing, and servicing medical devices for human use. Ordinarily, manufacturers undergo periodic FDA inspections to ensure compliance with 21 CFR 820.
Many of the FDA 21 CFR Part 820 provisions pertain to record keeping. Some obligate manufacturers to maintain records of document changes, document instructions for production processes, and to monitor process parameters. Also covered is training. Manufacturers must show they have procedures for identifying training needs and ensuring employees are trained well enough to perform their jobs.
Other FDA 21 CFR Part 820 provisions cover procedures for documenting changes to specifications, methods, processes, and procedures. Covered too are corrective and preventive action (CAPA) procedures that kick in when manufacturers notice a problem with their product, processes, or quality system. Ditto for handling complaints; manufacturers have to maintain a formal means of receiving, reviewing, and evaluating complaints and a way of tracking products that don’t meet their specs. (There is, however, a proviso by the FDA that entities making ventilators during the emergency have a process in place for reporting “adverse events” per 21 CFR Part 803.)
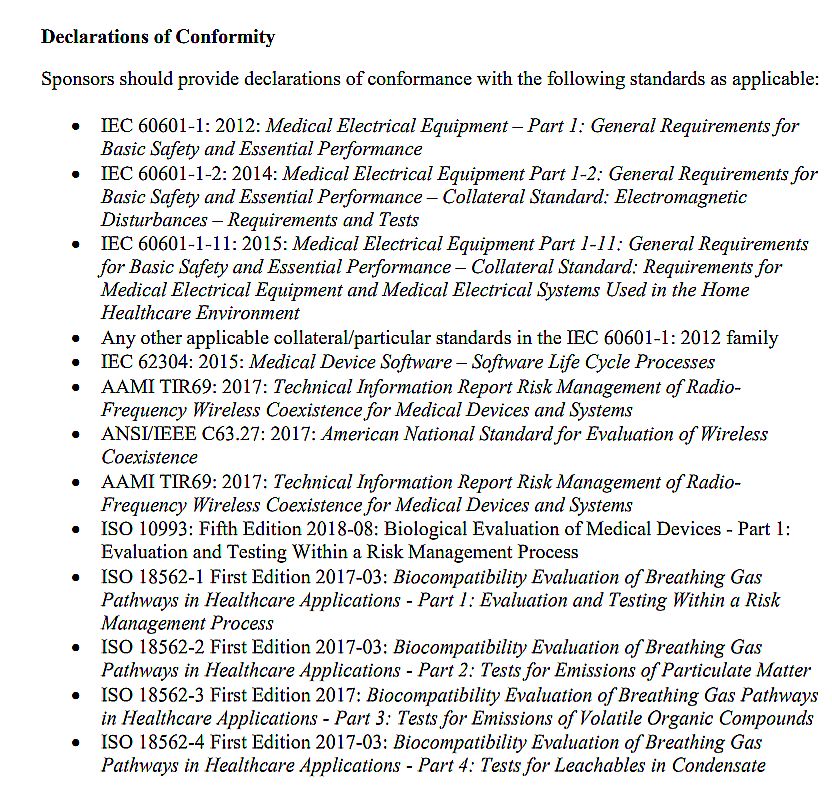
A partial list of standards that any ventilator produced during the emergency must meet.
The suspension of CGMP requirements during the crisis is one of the main reasons manufacturers such as GM can rapidly transition some of their production facilities to making ventilators. Left unsaid, at least as of this writing, is what happens to ventilators produced under these war-effort conditions once the pandemic is over. Whether they will be recalled, re-examined, or otherwise scrutinized is an open question.
Still, the FDA compels manufacturers making ventilators during the emergency to keep certain records and comply with labeling requirements. For example, manufacturers must track where the ventilators go and who distributes them.
Another important point to note is that the ventilator designs that will be made without CGMP dictates in place will necessarily be those that have already received FDA approval and have been in commercial use. The reason is that any devices made this way must meet safety, performance, and labeling requirements spelled out in a laundry list of international standards. The March 24 FDA document mentions 22 standards or paragraphs within standards. Among them are IEC 60601, the basic safety standard for medical equipment; IEC 62304, which covers software used in medical devices; ISO 18562, which covers the components in the ventilator breathing path; and numerous standards pertaining to RFI and EMI either originating from or potentially interfering with the ventilator electronics.
Of course, the only ventilator designs that can be easily demonstrated to meet these standards are those already sold commercially. This fact effectively eliminates the possibility of manufacturing any of the brand-new open-source designs now being proposed, even on an emergency basis.
All in all, the deck is stacked against well-meaning manufacturers interested in cranking out their own ventilator ideas. Instead, it might be useful to consider the advice from Michael Farrell, CEO of respirator maker ResMed: “We’ve got almost unlimited capacity to meet the needs of final manufacturing (of ventilators)….It’s not a final ventilator manufacturing problem. It’s a parts problem. We have over 500 parts going into these advanced invasive and non-invasive ventilators. As people come to help, we tell them, ‘Don’t buy the parts that we can use to make these at scale, help us make the parts.’ “
You may also like:
Filed Under: Fighting COVID-19